On the origin of cancer: studying somatic evolution in normal tissues
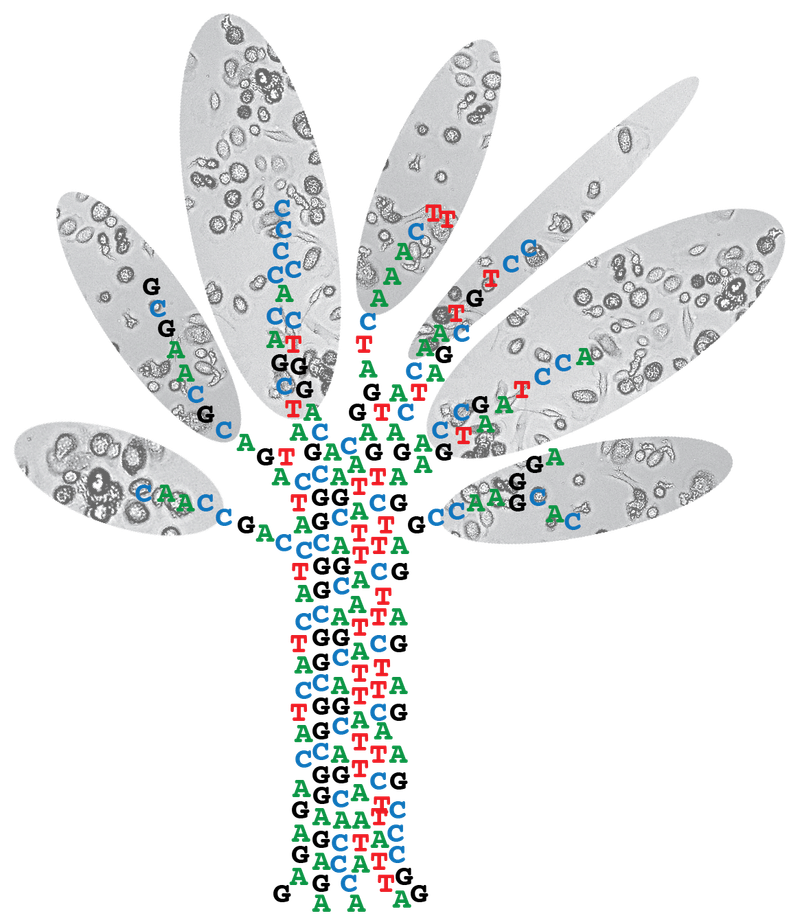
Mutation accumulation in normal cells is required for the development of cancers. Because aging is the biggest risk factor for cancer, it is thought that mutation accumulation is rate limiting for disease initiation. Indeed, as our cells age, they gradually accumulate mutations in their genomes. If a cell by chance acquires a bad mutation at the wrong time and place, malignant transformation can be triggered. According to this model, we should target these mutations, or their functional effects, in order to remove the driving force of the cancer and kill it.
However, with the recent developments of sequencing normal, noncancerous cells, we see that the mutation loads in normal tissues are already so high that it is very likely that there are always cells in our bodies with the right set of mutations, which are required for malignant transformation; yet we don’t have cancer. For example, in quite some newborns we can detect leukemia-driving fusion genes in their blood, yet these babies are perfectly healthy and do not develop leukemia. In addition, for certain cancer types, such as leukemia, young children show a higher incidence compared to young adolescents. This phenomenon represents an apparent paradox, as young cells should have less somatic (oncogenic) mutations than adult cells. It is very likely that mutation accumulation, although very necessary, is not the rate limiting step in cancer development.
Why then, do certain individuals develop cancer and others don’t? If mutation accumulation is not rate limiting for disease development, what is? And more importantly, shouldn’t we be targeting those rate limiting factors? In other words, if getting cancer is default, because of the relatively high mutation burden in normal tissues, how do our bodies keep the initiation of cancer in check and why does this sometimes fail?
Pinpointing the rate limiting steps in cancer initiation is challenging as many factors can play a role: ecological features within the various tissues, tissue damage responses, age, carcinogenic exposure, etc. Still, an increased understanding in how the body can keep cancer in check might revolutionize how we battle the disease: we have “stolen” our best ideas from nature, so why not this?
To answer these questions, we have 3 research themes in our lab.
Theme 1: Tissue-specific mutation accumulation in human stem cells
Theme 2: Tracking the origin of cancer
Theme 3: The etiology of therapy-related malignancies in cancer survivors


